Many people are diagnosed with a penicillin allergy in early childhood based on a rash or other non-specific symptoms. There can be several non-allergic causes for a rash such as a viral infection which may be misinterpreted as an allergic reaction. Less than 10% of all people who report a penicillin allergy are truly allergic. Of those who are truly allergic to penicillin, over 80% will lose their allergic tendency over a period of ten years. These facts highlight the need for identification of a true allergy to penicillin because they remain the antibiotic of choice for many infections. People who are unnecessarily designated as “penicillin allergic” may receive alternative antibiotics that cause more side effects, may be more costly and overall contribute to antibiotic resistance.
Why is penicillin important?
Penicillin family antibiotics are commonly used to treat a variety of bacterial infections including pneumonia, sinusitis, throat and ear infections. People who are listed as ‘penicillin allergic’ often receive broad-spectrum antibiotics which are stronger antibiotics than needed. Using broad spectrum antibiotics can lead to longer hospital stays, treatment failures, increase healthcare costs and infections such as Clostridium difficile associated with severe diarrhea. Unnecessary or excessive use of broad-spectrum antibiotics can also contribute to development of resistant “super bugs.” A careful evaluation can determine the status of your child’s penicillin allergy and help identify an antibiotic that will be safe and effective.
What are the signs and symptoms of a penicillin allergy?
An immediate allergic reaction to penicillin typically occurs quickly, usually within an hour after receiving the medication. It can occur in people who previously tolerated penicillin without any issues. Symptoms frequently involve the skin and include:
- Hives (also known as welts or urticaria, a raised, itchy rash)
- Swelling (also known as angioedema, commonly occurring on the face or tongue)
These reactions usually respond to an antihistamine and occasionally may require a dose of oral or injected corticosteroid.
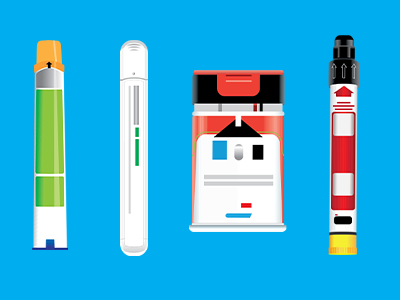
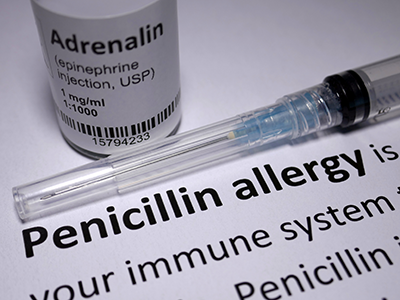
In rare cases, more serious reactions such as anaphylaxis can occur. The symptoms of anaphylaxis can include:
- Swelling of the tongue or throat
- Respiratory symptoms such as difficulty breathing, coughing, chest tightness, wheezing
- Abdominal symptoms such as cramping, vomiting or diarrhea
- Light-headedness or loss of consciousness caused by low blood pressure
These symptoms require immediate treatment with epinephrine, which can be administered with an autoinjector if available, and/or at the nearest emergency room or by Emergency Medical Service providers. Additional treatments may include inhaled albuterol to treat respiratory symptoms and intravenous fluids.
How is a penicillin allergy diagnosed?
A penicillin allergy can be evaluated by an allergist. During the initial visit, the provider will obtain a careful history and determine if penicillin skin testing and/or a penicillin challenge is required for the diagnosis.
What is penicillin skin testing?

Penicillin skin testing. Top image: skin prick testing. Bottom image: intradermal testing.
Penicillin skin testing is a highly reliable method to test for an IgE-mediated allergy to penicillin and is performed in children who developed symptoms consistent with allergic reactions after receiving a penicillin family antibiotic. If indicated, the child will return for a separate penicillin skin testing appointment. This is a two part test. The first step involves skin prick testing with two forms of penicillin. If this test is negative, then a small amount of penicillin is injected under the skin for intradermal testing.
If both tests result negative, it is highly unlikely that the child has a penicillin allergy. The child will then receive a one-time dose of amoxicillin (type of penicillin) and will be monitored in the office to ensure no reaction develops. If the oral challenge test dose is tolerated without a reaction after negative skin testing, the child is determined to not be allergic to penicillin. If skin testing is positive and the child requires penicillin, an allergist can assist with alternatives or discuss drug desensitization. The desensitization procedure can be performed under the supervision of an allergist for temporary, but safe use of the medication. Penicillin desensitization is only performed when there is a clear benefit to using penicillin for an infection.
What is a penicillin challenge?
If the provider determines that the child is at low risk for having a true allergy to a penicillin family antibiotic, then the child will be scheduled for an in-office medication challenge. During this challenge, the antibiotic in question will be introduced without prior skin testing followed by observation time. If the antibiotic is tolerated, then the child is not at risk for a serious immediate allergic reaction to the antibiotic in question. This process typically requires 2-3 hours.
My child might have or has been diagnosed with penicillin/penicillin family antibiotic allergy. What should I do next?
Even if you think that your child is allergic to penicillin or a penicillin family antibiotic, allergies can change over time. You can schedule a consultation with an allergist/allergy provider to determine if your child is eligible for penicillin testing and an oral challenge.
References:
-
- Penicillin Allergy: Are You Allergic to Penicillin? Information for patients and families. Duke Asthma, Allergy, and Airway Center (Images/Data used by permission)
- Drug Allergy: an updated practice parameter. Ann Allergy Asthma Immunolo. 2010 Oct: 105(4): 259-273
- Penicillin Allergy FAQ
 https://riseandshine.childrensnational.org/wp-content/uploads/2023/08/allergy-causing-foods-feature.png
300
400
Rise and Shine
https://riseandshine.childrensnational.org/wp-content/uploads/2017/11/childrens_riseandshine_logo.jpg
Rise and Shine2023-08-31 11:30:132023-08-31 11:38:06Introducing food allergens to your baby
https://riseandshine.childrensnational.org/wp-content/uploads/2023/08/allergy-causing-foods-feature.png
300
400
Rise and Shine
https://riseandshine.childrensnational.org/wp-content/uploads/2017/11/childrens_riseandshine_logo.jpg
Rise and Shine2023-08-31 11:30:132023-08-31 11:38:06Introducing food allergens to your baby



 Joel Brooks, DO, was a staff allergist in the Division of Allergy and Immunology at Children’s National Hospital.
Joel Brooks, DO, was a staff allergist in the Division of Allergy and Immunology at Children’s National Hospital.
















Leave a Comment
Want to join the discussion?Feel free to contribute!