The prevalence of food allergy is increasing. Various theories exist about why, including the hygiene hypothesis (early life exposure to bacteria may alter the immune response and be protective against allergy), changes in dietary habits (vitamin D, antioxidants), food processing practices and timing of introduction of foods1.
Preventing food allergy
Recent studies have shown that children at risk for peanut allergy have a reduced risk of developing peanut allergy if peanut is introduced early2,3 . The Learning Early About Peanut (LEAP) trial showed that early introduction of peanut significantly reduces the risk of peanut allergy up to 80% in children at high risk of developing a peanut allergy (those with severe eczema and/or egg allergy)2. Guidelines recommend that if an infant (4-6 months of age) has severe eczema or egg allergy, their pediatrician can screen for peanut allergy with a blood test or refer the child to an allergist for evaluation and possible testing prior to introduction4.
For foods other than peanut and egg, the evidence is not as strong that early introduction reduces the risk of food allergy, but some studies suggest that early introduction of cow’s milk and cashew may help prevent these food allergies5,6. One study looked at the early introduction of multiple foods into an infant’s diet (peanut, cooked egg, cow’s milk, sesame, whitefish, and wheat) but the adherence to this diet was difficult for the participants given the need to feed infants multiple foods at an early age3 . The safety of early introduction has been confirmed in these studies2,3,5,6 .
Given these findings, allergists often encourage early introduction of egg and peanut to help prevent food allergy, and introduction of the other common allergenic foods (milk, wheat, sesame, tree nuts, fish, shellfish) as soon as the family can, in alignment with what is culturally and developmentally appropriate.
Allergy testing prior to introduction is determined necessary or unnecessary through conversations with the family and their pediatrician and/or allergist. It is important that families to keep up with routine physicals so they can have these discussions with their medical provider. During COVID there are alternative options to in-person visits like telehealth visits.
Diagnosis and management of food allergies
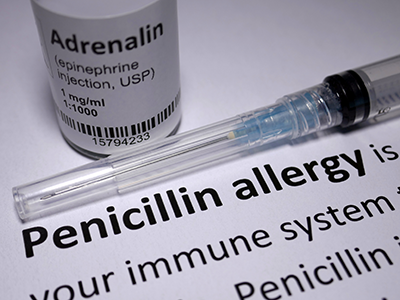
One in thirteen kids have food allergy7. A food allergy is when the immune system recognizes a food as an allergen and results in an allergic reaction after your child eats that food. Allergic reaction symptoms include hives, swelling, itching, runny nose, congestion, cough, difficulty breathing, vomiting, stomachache, dizziness and fainting.
History is key in the diagnosis of food allergy — What did they eat? What symptoms occurred? How soon? Have they eaten this food before or afterward? If so, what happened? Skin prick tests and blood (food specific IgE) tests are adjuncts to help determine food allergy and an oral food challenge is the gold standard test.
We avoid food panel testing because these tests can result in false positives and induce anxiety in parents and/or lead to inappropriate food restriction diets. For example, your child was tested to multiple foods and wheat came back positive, but they eat wheat-based pasta without any reactions — hence, they do not have a wheat allergy and they do not need to avoid it!
There are other food allergies such as food protein induced enterocolitis syndrome (FPIES) that are diagnosed based on a history of delayed repetitive vomiting and eosinophilic esophagitis (EoE) that requires an endoscopy and biopsy by a GI physician for diagnosis. Food sensitivity tests (IgG) are not scientifically-proven and not indicated for diagnosis.
The mainstay of treatment for food allergy is avoidance and carrying epinephrine autoinjectors at all times. Avoidance includes reading labels and avoiding warning labels due to risk of cross-contamination.
Recently, a peanut oral immunotherapy (OIT) drug was FDA-approved for children and teens 4-17 years old. This drug is not curative but indicated to reduce the risk of a severe allergic reaction in the case of an accidental exposure. Families should discuss side effects, risks and benefits, and their goals for this treatment to see if your child would be a good candidate for this drug.
References
- Sicherer SH, Sampson HA. Food allergy. J Allergy Clin Immunol. 2010 Feb;125(2 Suppl 2):S116-25. doi: 10.1016/j.jaci.2009.08.028. Epub 2009 Dec 29. PMID: 20042231.
- Du Toit G, Roberts G, Sayre PH, Bahnson HT, Radulovic S, Santos AF, et al. Randomized Trial of Peanut Consumption in Infants at Risk for Peanut Allergy. N Eng J Med. 2015;372:803-813.
- Perkin MR, Logan K, Marrs T, Radulovic S, Craven J, Flohr C, Lack G; EAT Study Team. Enquiring About Tolerance (EAT) study: Feasibility of an early allergenic food introduction regimen. J Allergy Clin Immunol. 2016 May;137(5):1477-1486.e8. doi: 10.1016/j.jaci.2015.12.1322. Epub 2016 Feb 17. PMID: 26896232; PMCID: PMC4852987
- Togias A, Cooper SF, Acebal ML, Assa’ad A, Baker JR, Jr., Beck LA, et al. Addendum guidelines for the prevention of peanut allergy in the United States: Report of the National Institute of Allergy and Infectious Diseases-sponsored expert panel. J Allergy Clin Immunol. 2017; 139(1):29-44.
- Sakihara T, Otsuji K, Arakaki Y, Hamada K, Sugiura S, Ito K. Randomized trial of early infant formula introduction to prevent cow’s milk allergy. J Allergy Clin Immunol. 2020;0nline ahead of print.
- Peters RL, Barret DY, Soriano VX, McWilliam V, Lowe AJ, Ponsonby AL, et al. No cashew allergy in infants introduced to cashew by age 1 year. J Allergy Clin Immunol. 2020;0nline ahead of print.
- Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics. 2009 Dec;124(6):1549-55. doi: 10.1542/peds.2009-1210. Epub 2009 Nov 16. PMID: 19917585.
 https://riseandshine.childrensnational.org/wp-content/uploads/2023/11/ketogenic-foods-feature.png
300
400
Rise and Shine
https://riseandshine.childrensnational.org/wp-content/uploads/2017/11/childrens_riseandshine_logo.jpg
Rise and Shine2023-11-16 15:06:312023-11-16 15:15:01Using ketogenic diets to manage seizures
https://riseandshine.childrensnational.org/wp-content/uploads/2023/11/ketogenic-foods-feature.png
300
400
Rise and Shine
https://riseandshine.childrensnational.org/wp-content/uploads/2017/11/childrens_riseandshine_logo.jpg
Rise and Shine2023-11-16 15:06:312023-11-16 15:15:01Using ketogenic diets to manage seizures



















Leave a Comment
Want to join the discussion?Feel free to contribute!